Understanding Type 1 Diabetes & Type 2 Diabetes
Diabetes is not a single disease, rather a collective name for different conditions that lead to an elevation in blood glucose levels. It is a chronic disease, that is preventable, manageable, but full-blown diabetes is not curable. Depending on the causes and clinical picture, there are several types of diabetes. However, two of the sub-types are most common. 5-7% of those living with diabetes belong to type 1 diabetes, and around 90% belong to type 2 diabetes, other types are extremely rare. Thus mostly when people say diabetes or sugar disease, they are mostly talking about the so-called type 2 diabetes.
Diabetes a major health challenge in India
Diabetes is epidemic in India, and undoubtedly one of the most common diseases. It is estimated that there were around 72 million people living with diabetes in India in 2017. This figure is expected to almost double by 2045. At present nearly half of those with diabetes do not know about it, that is due to lack of monitoring of blood glucose in India, although awareness is fast rising. Further, statistics indicate that those living in bigger cities are at higher risk than those living in rural areas due to dietary and physical activity differences.
Indian physicians were perhaps one of the first to describe diabetes and its two sub-types in details. Yes, diabetes was quite prevalent in India even 3000 years back. Thus Charak and Sushruta somewhere between 400-500 A.D. identified that there was diabetes of thin (type 1), and another kind of diabetes affecting overweight people (type 2). They came up with several herbal remedies that are used in India to date.
The ancient name for diabetes in India is Madhumeha. Madhumeha means sweet urine as early Indians noticed that ants were attracted to the place of urinating in diabetes. Europeans also knew that in diabetes urine becomes sweeter, and for long urine sugar tests were standard in the diagnosis of diabetes.
There are several types of diabetes, but we look at the two most common types.
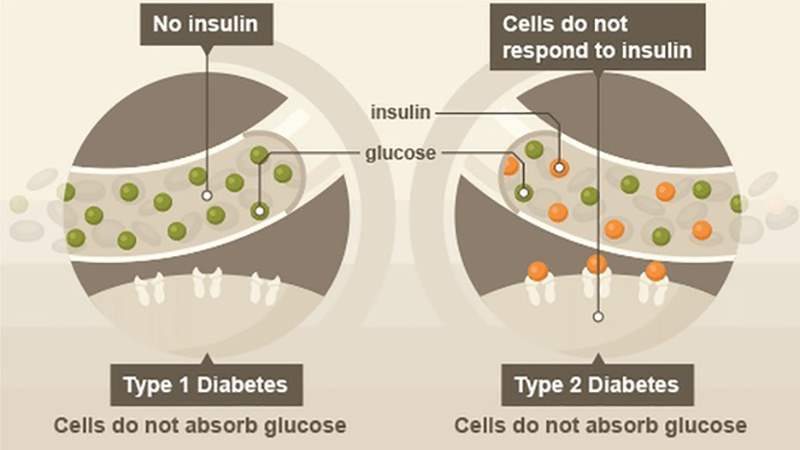
Type 1 diabetes
Type 1 diabetes is called the diabetes of lean and young, because it is diagnosed at a young age and most people affected by it are not obese. It is not uncommon for this type of diabetes to be diagnosed at school age. It usually starts quite suddenly. Thus the symptoms may be severe abdominal pain, nausea, increased thirst, increased passing of urine, fruity smell from mouth. Doctors may sometimes confuse it with other diseases or infections.
It is an autoimmune disease, a condition when our immune system stops recognizing the insulin-producing beta cells in the pancreas and start attacking them, thus killing them in process. By the diagnosis time of person, there is an acute deficit of insulin and loss of most of the beta cells happens.
The diagnosis of this type of diabetes is common because of hospitalization, resulting from complications and missed diagnoses.
In type 1 diabetes, insulin is the only treatment.
Type 2 diabetes
It is the most common type, almost 90% of cases belong to this type. Thus if you know anyone living with diabetes, he or she probably belongs to this type.
This type of diabetes is rare in young age; diagnosis of it happens mostly in the 30s or even later. It develops gradually, and in most cases over several years. However, people are not able to identify it in early stages. It is reversible in some cases, as in most cases there are no early symptoms.
Faulty lifestyle causes type 2 diabetes, wrong dietary habits and lack of exercise are the primary culprits. It is more about insulin resistance, rather than insulin deficit. It means that in early stages a person has enough insulin in blood but body tissues fail to react to insulin as they have become resistant to it.
Increased thirst, appetite, and urination are common symptoms of type 2 diabetes. You will often diagnose it by chance during regular health checkup, as many people fail to listen to their body. Other symptom commonly found in type 2 is chronic fatigue without any reason. Some people may already have complications at the time of diagnosis like weakened eyesight (due to diabetic retinopathy), a disease of peripheral nerves (altered sensation).
This type of diabetes is mostly treated with oral pills. In later stages, when there is insulin deficit along with insulin resistance, your doctor will add insulin therapy.
Monitoring blood glucose – an essential element of diabetes care
Though people living with diabetes fully understand the need of taking medications regularly. However, in resource-limited setting people often tend to neglect the importance of regular self-glucose monitoring. In fact, in countries like India, even physicians fail to educate patients about the importance of blood glucose monitoring.
Lab blood glucose tests are useful, but nothing can replace the data gathered through regular self-monitoring as it can show a much clearer picture.
Two important readings to pay attention to are: fasting blood glucose levels and postprandial blood glucose. Fasting blood glucose monitoring has to do in the morning, on an empty stomach. For accurate results fasting glucose has to check 8-12 hours post-dinner. If you give too much interval, readings may be faulty (let’s say after 14 hours of last meal). You have to check postprandial blood glucose between one to two hours of starting the meal.
Fasting blood glucose levels show how accurately one is controlling the blood sugar, and it also says about the effectiveness of medications. However, postprandial readings are very important as they say about the spikes. One should check the postprandial level after breakfast, lunch, and dinner or at least once after the most substantial meal. Now it is very clear that postprandial spikes are responsible for many complications.
Thus remember to check your blood glucose regularly at home, and remember that self-monitoring has its value. Blood glucose monitoring is as necessary as taking medications daily for managing type 1 diabetes & type 2 diabetes.